Evidence-based dietary interventions in psychiatric disorders
Epidemiological studies indicate that diet has a significant impact on mental health, and nutritional interventions can contribute to improvements in psychological well-being.
Epidemiological studies are a type of scientific research that examines how various factors (e.g. diet, lifestyle, environment) affect human health.
Thanks to these studies, researchers can observe, for example, that people who follow certain eating patterns – such as the Mediterranean diet – are less likely to suffer from depression compared to those who consume large amounts of fast food and processed foods.
Evidence-based dietary interventions are approaches to changing one’s diet that have been thoroughly studied and proven effective in improving mental health. This means that researchers have conducted experiments and compared different groups of people to determine whether dietary changes genuinely help reduce symptoms, such as those of depression.
An example of such an intervention is adopting a diet rich in vegetables, fruits, fish, nuts, and olive oil—foods known to positively influence brain function and well-being. Studies show that individuals who follow a healthy diet are less likely to experience depression and anxiety compared to those who consume large amounts of simple sugars and saturated fats (Grajek et al., 2022).
A challenge for researchers remains the need to conduct more rigorous, evidence-based studies that can clearly define the role of diet in the prevention and treatment of mental disorders (Grajek et al., 2022).
Dietary interventions with proven preventive effects in mental illnesses
Mediterranean diet
The Mediterranean diet is one of the most thoroughly researched dietary patterns, known for its beneficial effects on health—including mental health. It is based on the traditional eating habits of people living in countries bordering the Mediterranean Sea, such as Greece, Italy, and Spain. The core principles of this diet include:
- High consumption of vegetables, fruits, legumes (e.g. beans, lentils, chickpeas), nuts, and wholegrain cereals (e.g. wholemeal bread, brown rice, wholewheat pasta).
- Healthy fats, primarily from olive oil.
- Regular intake of fish and seafood, which are rich sources of valuable omega-3 fatty acids.
- Moderate consumption of red wine, typically with meals and by adults.
- Low intake of red meat and highly processed foods, such as fast food, sweets, and crisps (Grajek et al., 2022).
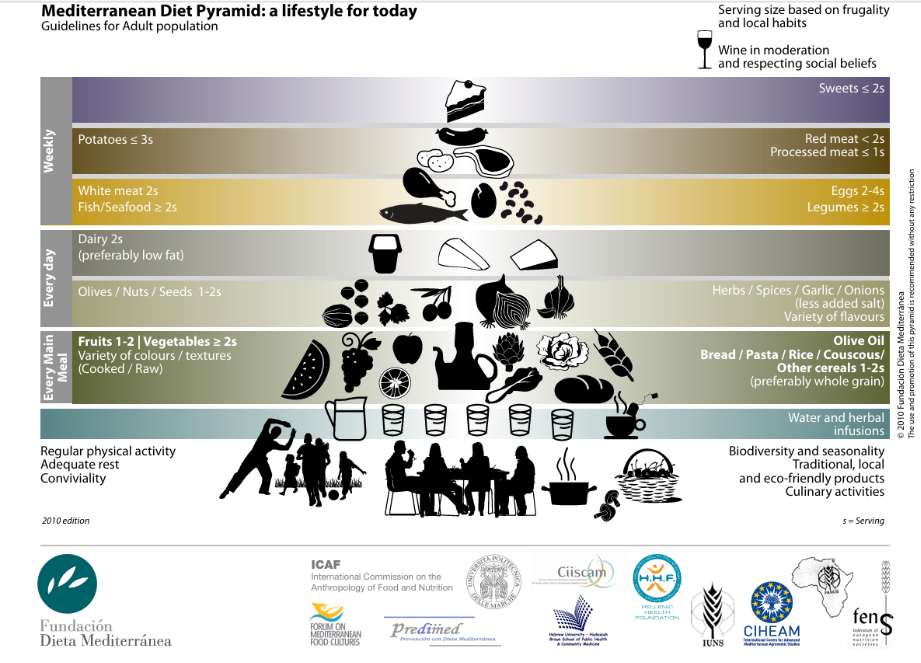
In the illustration below, the core principles of the Mediterranean diet are presented. This graphic can be used for educational purposes when working with clients and can be downloaded from the following website: https://dietamediterranea.com/en/nutrition/
The pyramid is available in various languages, including Arabic, Spanish, Catalan, Basque (Euskera), French, Galician, Greek, English, Italian, and Portuguese.
Characteristics of Selected Food Products of the Mediterranean Diet
| Product/Product Group | Properties | Recommendations |
| Olive Oil | • Extra virgin olive oil is a source of antioxidant and anti-inflammatory substances: tocopherols, polyphenols, and phytosterols, as well as monounsaturated fatty acids. • Refined olive oil (with a similar amount of monounsaturated fats) loses most of these beneficial substances during processing and is less valuable nutritionally. | • Consume olive oil (preferably extra virgin) raw whenever possible. • Add it to vegetables, legumes, salads, and other dishes. • Olive oil is considered a processed product, but it’s only one component of a balanced diet. |
| Vegetables | • Vegetables are a source of dietary fiber, vitamins, and antioxidant compounds (e.g. vitamin C, beta-carotene, lycopene, flavonoids, isothiocyanates). | • Eat vegetables as often as possible. Ideally, include them in most meals throughout the day. • Try to eat at least one portion of raw vegetables daily. • Prefer seasonal and colorful vegetables (varied colors = varied antioxidants). |
| Fruits | • Fruits are a source of dietary fiber, vitamins, and antioxidant compounds (e.g. vitamin C, beta-carotene, vitamin E, flavonoids, chlorogenic acid). • Due to their natural sugar content, consume them in smaller quantities. | • Eat fresh, raw fruits daily, e.g. as dessert. • Try to eat 1–2 servings of fresh fruit per day. • Ensure variety and seasonality. |
| Whole Grains | • Whole grain products are a source of dietary fiber, B vitamins, and many minerals. • Fiber increases satiety, regulates bowel movements, modulates gut microbiota, limits cholesterol absorption, and positively affects post-meal glycemia. | • Choose whole grain bread, whole wheat pasta, coarse groats, brown rice, and whole grain flour. |
| Legumes | • Legumes are a source of plant protein, dietary fiber, vitamins, and minerals. | • Eat 3 servings of any type of legumes per week, e.g. lentils, beans, chickpeas, soy. • Replace meat with legumes. |
| Fish & Seafood | • Fish and seafood are sources of protein, omega-3 fatty acids, selenium, iodine, and zinc. • Omega-3 fatty acids have anti-inflammatory properties. They must be supplied with the diet because the body cannot synthesize them. | • Aim to eat: 1 serving per week of lean white fish (e.g. cod, flounder, perch); 2 servings per week of fatty fish (e.g. mackerel, salmon, herring, sardines); occasional shellfish (e.g. oysters, mussels, squid, shrimp). |
| Dairy Products | • Dairy is a source of protein and calcium. • Fermented dairy products provide probiotics that positively affect the gut. • Calcium in dairy is well absorbed and is a key component of bones. | • Consume 2 servings of dairy daily. • Choose natural, fermented dairy products. • Yogurt can be combined with fruits and nuts. |
| Nuts, Seeds | • Nuts and seeds are rich in healthy fats, fiber, vitamins, and minerals (e.g. selenium, magnesium, zinc, copper, potassium). • They provide essential fatty acids (including omega-3), fiber, and some protein. | • Eat a handful of nuts daily or 3 servings weekly as a healthy snack alternative (1 serving ≈ 30 g). • Choose: walnuts, almonds, hazelnuts, seeds (pumpkin, sunflower). |
The Mediterranean diet vs. the Western diet
The Mediterranean diet and the Western diet differ significantly – both in terms of ingredients and their impact on health. The Mediterranean diet is based on natural, unprocessed foods and includes large amounts of vegetables, fruits, wholegrain cereals, nuts, seeds, and legumes. Its primary fat source is olive oil, and its main protein sources are fish and poultry. In contrast, the Western diet – common in developed countries – is rich in ultra-processed foods, such as ready-made meals, fast food, sweets, salty snacks, and fizzy drinks. It is dominated by red and processed meats, high levels of saturated and trans fats, salt, and simple sugars. The health effects of these diets also differ. The Mediterranean diet supports mental well-being and reduces the risk of depression, thanks to its anti-inflammatory components and nutrients that support brain function. The Western diet has the opposite effect – it increases the risk of heart disease, obesity, and depression due to its pro-inflammatory properties and negative impact on the nervous system (Zielińska et al., 2022).
To help better understand the differences between the Mediterranean and typical Western diets, a visual comparison in the form of inverted food pyramids has been prepared. The illustration below clearly and simply shows which food groups should dominate the daily diet and which should be limited in order to support both mental and physical health. This graphic can be a valuable educational tool – especially in one-to-one work with clients – as it helps to visually explain how to change dietary habits to eat more mindfully and in a way that benefits the body.
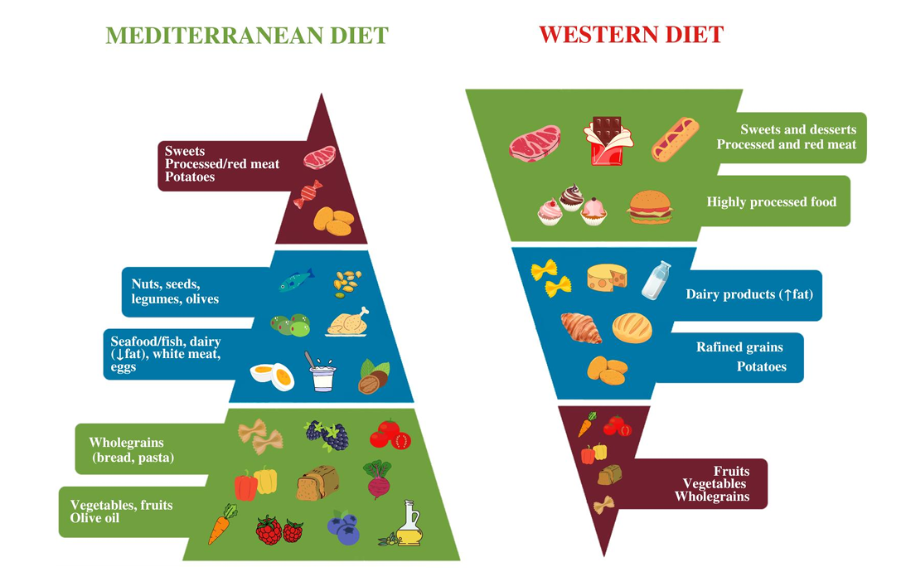
Source: Zielińska et al. (2022)
The following quiz is educational and indicative in nature – it is not a diagnostic or medical tool. Its purpose is to encourage reflection on your own eating habits and highlight areas where you may consider making positive changes.
The results of the quiz do not replace consultation with a dietitian, psychologist, or doctor. If you have any concerns about your health or diet, please seek advice from a qualified specialist.
The quiz can be a helpful prompt for reflecting on whether it might be worth, for example:
– increasing your intake of vegetables and wholegrain products,
– reducing ultra-processed foods and simple sugars,
– paying more attention to regular meals and proper hydration.
Take the quiz and discover which of your everyday habits might need adjusting – not only to support your physical health, but your mental well-being too.
INTERACTIVE ACTIVITY 24

Does the Mediterranean diet help in treating depression?
A research team led by Parletta (2019) set out to investigate whether following the Mediterranean diet combined with fish oil supplementation could improve mental health in individuals experiencing depression. The study included 152 adults (aged 18–65) showing symptoms of depression. Participants were divided into two groups:
- Mediterranean diet group – for three months, they received food hampers and took part in cooking workshops, and for six months, they took fish oil supplements.
- Control group – took part in social gatherings but made no changes to their diet.
The results were clear: participants following the Mediterranean diet began eating more vegetables, fruits, nuts, and wholegrain products, while reducing their intake of red meat and unhealthy snacks. After three months, their mental health improved—depression symptoms decreased, and quality of life increased. Moreover, the positive effects were still observed after six months.
The most significant improvements in well-being were associated with higher intake of nuts, vegetables, and a greater variety of vegetables. Better mental health was also linked to increased omega-3 levels and decreased omega-6 levels in the blood.
Which components of the Mediterranean diet may improve mental health?
- Vegetables and fruits – rich in vitamins and antioxidants that protect nerve cells.
- Nuts – high in healthy fats and minerals that support brain function.
Omega-3 fatty acids – found in fish, plant oils, and nuts; they help regulate mood and reduce inflammation in the body.
The study presented shows that adopting a healthier diet is achievable and that the Mediterranean diet, combined with fish oil supplementation, can benefit individuals with depression. It also suggests that improvements in mental health may result from increased intake of healthy fats, vegetables, and other natural foods.

The Mediterranean diet and the risk of depression
Bizzozero-Peroni et al. (2025) aimed to determine whether following the Mediterranean diet could effectively reduce symptoms of depression in adults. While earlier studies had suggested that people adhering to this diet were less likely to develop depression, it was still unclear whether a dietary intervention could genuinely help those already experiencing depressive symptoms.
The researchers analysed five clinical trials involving 1,507 participants aged 22 to 53, all diagnosed with depression or experiencing mild to moderate depressive symptoms. They compared the effects of the Mediterranean diet with control groups that did not follow this diet.
The findings revealed that the Mediterranean diet significantly reduced depressive symptoms among young and middle-aged adults with mild to moderate depression. On average, those following the diet experienced a 53% reduction in the severity of depressive symptoms compared to the control group.
While the Mediterranean diet appears to hold strong potential in alleviating depressive symptoms, larger and longer-term studies are needed to confirm these effects definitively. At present, the diet should not be considered a stand-alone treatment for depression, but it may serve as a valuable complement to conventional therapies.
An analysis of four long-term studies (spanning 10 years) showed a 33% lower risk of depression in individuals who followed the Mediterranean diet (Lassale et al., 2019).
The Mediterranean diet and anxiety disorders
Some studies suggest that this way of eating may also offer protection against anxiety disorders; however, there is still a lack of conclusive scientific evidence confirming this effect. This means that while the diet may be helpful, it should not be considered a standalone method for treating anxiety (Madani et al., 2022).
The Mediterranean diet has well-documented benefits in supporting the treatment of depression.
- Evidence for its preventive role is promising but requires further research.
- It can be an effective complement to depression therapy, but it does not replace pharmacological treatment or psychotherapy.
There is no conclusive evidence supporting the effectiveness of the Mediterranean diet in treating anxiety disorders.
INTERACTIVE ACTIVITY 25
| Bibliography |
| Grajek, M., Krupa-Kotara, K., Białek-Dratwa, A., Sobczyk, K., Grot, M., Kowalski, O., & Staśkiewicz, W. (2022). Nutrition and mental health: A review of current knowledge about the impact of diet on mental health. Frontiers in Nutrition, 9, 943998. https://doi.org/10.3389/fnut.2022.943998 Parletta, N., Zarnowiecki, D., Cho, J., Wilson, A., Bogomolova, S., Villani, A., et al. (2019). A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutritional Neuroscience, 22(7), 474–487. https://doi.org/10.1080/1028415X.2017.1411320 Bizzozero-Peroni, B., Martínez-Vizcaíno, V., Fernández-Rodríguez, R., Jiménez-López, E., Núñez de Arenas-Arroyo, S., Saz-Lara, A., Díaz-Goñi, V., & Mesas, A. E. (2025). The impact of the Mediterranean diet on alleviating depressive symptoms in adults: A systematic review and meta-analysis of randomized controlled trials. Nutrition Reviews, 83(1), 29–39. https://doi.org/10.1093/nutrit/nuad176 Lassale, C., Batty, G. D., Baghdadli, A., et al. (2019). Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Molecular Psychiatry, 24, 965–986. https://doi.org/10.1038/s41380-018-0237-8 Madani, S., Ahmadi, A., Shoaei-Jouneghani, F., et al. (2022). The relationship between the Mediterranean diet and Axis I disorders: A systematic review of observational studies. Food Science & Nutrition, 10, 3241–3258. https://doi.org/10.1002/fsn3.2952 Zielińska, M., Łuszczki, E., Michońska, I., & Dereń, K. (2022). The Mediterranean diet and the Western diet in adolescent depression—Current reports. Nutrients, 14(20), 4390. https://doi.org/10.3390/nu14204390 |
MIND diet – how nutrition affects brain health
The MIND Diet (Mediterranean-DASH Diet Intervention for Neurodegenerative Delay) is a dietary approach that combines the benefits of the Mediterranean diet and the DASH diet (Dietary Approaches to Stop Hypertension). It was specifically designed to protect brain health and reduce the risk of neurodegenerative diseases such as Alzheimer’s disease (Grajek et al., 2022).
Key principals of the MIND diet:
✔️ High intake of leafy green vegetables (e.g. spinach, lettuce, kale), berries, nuts, wholegrain products, and olive oil;
✔️ Regular consumption of fish and poultry (e.g. chicken, turkey);
✔️ Limiting red meat, fried foods, sweets, and processed products




How does the MIND diet affect mental health?
The MIND diet was primarily developed to support memory and concentration, but research shows it may also help prevent depression and improve overall well-being (Grajek et al., 2022).
Preliminary studies have found that individuals who follow the MIND diet experience a slower decline in cognitive abilities as they age. Additionally, consuming berries and leafy green vegetables may enhance brain function. Scientific literature highlights that people adhering to the MIND diet are less likely to suffer from depression and mood disorders.
Compared to the Mediterranean and DASH diets alone, the MIND diet places greater emphasis on berries and leafy greens, while limiting fruit, dairy products, and potatoes (Grajek et al., 2022).
Compared to the Mediterranean and DASH diets, the MIND diet places greater emphasis on the consumption of berries and leafy green vegetables, while limiting the intake of fruits, dairy products, and potatoes (Grajek et al., 2022).

Can the MIND diet help treat depression in older adults?
Depression is a common issue among older adults, especially those with memory problems, a history of stroke, or vascular diseases. Researchers set out to examine whether diet could help reduce the risk of depression and support mental health (Cherian et al., 2021). To do so, they studied 709 individuals with an average age of 80.4 over a period of 6.5 years, tracking both their dietary habits and symptoms of depression. They assessed the impact of three healthy dietary patterns (DASH, MIND, and Mediterranean) compared to the Western diet, which is high in ultra-processed foods, sugar, and saturated fats.
What did the results show?
- People who followed the MIND or DASH diet experienced fewer symptoms of depression.
- Individuals following a Western-style diet had a higher risk of depression—the more fast food and sweets they consumed, the worse they felt.
The study demonstrated that diet can be an effective tool in reducing the risk of depression in older adults. Healthy dietary patterns – particularly the MIND and DASH diets – appear to have a positive impact on mental well-being, whereas the Western diet may worsen depressive symptoms.
Can the MIND diet help reduce stress and improve metabolic health?
Research suggests that the MIND diet not only supports brain function but may also help reduce stress and improve overall health—especially in individuals with obesity (Ardekani et al., 2023).
In a study by Ardekani and colleagues (2023), 339 adults aged 20–50 with obesity (BMI ≥ 30 kg/m²) took part. Participants completed a dietary questionnaire, and their adherence to the MIND diet was scored. Researchers then assessed not only their eating patterns but also health indicators such as stress levels, blood pressure, and insulin resistance (a key factor in the development of type 2 diabetes).
- Individuals who more closely followed the MIND diet consumed more brain-supportive foods such as vegetables, nuts, and wholegrains, and ate fewer sweets and baked goods compared to those with the lowest MIND scores.
- Participants with higher adherence to the MIND diet showed lower stress levels and better insulin sensitivity, suggesting a reduced risk of insulin resistance and diabetes.
This study suggests that following the MIND diet may help reduce stress and improve metabolic health, regardless of age, BMI index, gender, or physical activity level. Although originally developed to protect cognitive function, the MIND diet appears to have broader health benefits – particularly for individuals with obesity.
Challenges in following the Mediterranean diet among individuals with depression
Research shows that the Mediterranean diet can help in managing depression, but following it is not always easy. Açik et al. (2024) investigated the difficulties faced by people with a clinical diagnosis of depression who followed the Mediterranean diet for 12 weeks.
Positive aspects reported:
- Acceptance of the taste of most meals
- Increased motivation to continue the diet after the study
- Reduction in depressive symptoms
Main challenges identified:
- High cost of foods recommended in the Mediterranean diet
- The time commitment required to prepare meals
- Negative attitudes from family and friends, which made adherence more difficult
Although the Mediterranean diet may help reduce depressive symptoms, its practical implementation can be hindered by various obstacles. The biggest challenge turned out to be social pressure and lack of support from one’s immediate environment. Researchers suggest that future efforts should focus on better understanding how social support from family and friends can help sustain healthy eating habits.
- The MIND diet combines the benefits of the Mediterranean and DASH diets, supporting brain health.
- It may reduce the risk of depression and improve well-being, especially in older adults.
- It helps in reducing stress and improving metabolic health.
- Younger individuals may face challenges in following it, but they can benefit from support in changing their eating habits.
INTERACTIVE ACTIVITY 26
| Bibliography |
| Grajek, M., Krupa-Kotara, K., Białek-Dratwa, A., Sobczyk, K., Grot, M., Kowalski, O., & Staśkiewicz, W. (2022). Nutrition and mental health: A review of current knowledge about the impact of diet on mental health. Frontiers in Nutrition, 9, 943998. https://doi.org/10.3389/fnut.2022.943998 Cherian, L., Wang, Y., Holland, T., Agarwal, P., Aggarwal, N., & Morris, M. C. (2021). DASH and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diets are associated with fewer depressive symptoms over time. The Journal of Gerontology: Series A, 76(1), 151–156. https://doi.org/10.1093/gerona/glaa044 Ardekani, A. M., Vahdat, S., Hojati, A., Moradi, H., Tousi, A. Z., Ebrahimzadeh, F., & Farhangi, M. A. (2023). Evaluating the association between the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet, mental health, and cardio-metabolic risk factors among individuals with obesity. BMC Endocrine Disorders, 23(1), 29. https://doi.org/10.1186/s12902-023-01284-8 Açik, M., Bayindir Gümüş, A., Ekici, A., Çağiran Yilmaz, F., & Küçüksu, M. (2024). Mediterranean-DASH diet intervention for neurodegenerative delay diet and psychological problems in maintenance hemodialysis patients by the structural equation modeling analysis of malnutrition and inflammation markers approach. Journal of Renal Nutrition. Advance online publication. https://doi.org/10.1053/j.jrn.2024.09.006 |
Ketogenic diet
Can the ketogenic diet help in treating depression and other mental disorders?
Researchers are increasingly exploring the impact of diet on mental health. One particularly interesting approach is the ketogenic diet, which has long been used in the treatment of epilepsy and is now showing potential benefits for individuals with serious mental health conditions such as depression, bipolar disorder, and schizophrenia (Danan et al., 2022; Grajek et al., 2022).

What is the ketogenic diet?
The ketogenic diet is a way of eating that is based on very low carbohydrate (sugar) intake and high fat consumption. As a result, the body begins to use fat as its primary source of energy instead of glucose. In a typical diet, carbohydrates (such as bread, pasta, fruit, and potatoes) are the main source of energy. In contrast, the ketogenic diet shifts the body into a state called ketosis, where it starts producing ketones – compounds made from fat that replace sugar as fuel for the brain and muscles. This process helps to stabilise blood glucose levels and improves the body’s ability to regulate energy metabolism (Grajek et al., 2022).
The ketogenic diet as a support in treating severe psychiatric disorders
Danan et al. (2022) conducted a study involving 31 adult patients hospitalised in a psychiatric facility. These individuals had severe mental disorders and had not responded well to standard treatments, such as medication and psychotherapy. As part of the intervention, a ketogenic diet was introduced to their treatment plan. This meant consuming very few carbohydrates—no more than 20 grams per day. Such a diet forces the body to burn fat instead of carbohydrates, leading to a metabolic state called ketosis.
The study has shown that improvement was observed in the individuals following the rules of ketogenic diet:
- Depressive symptoms significantly decreased – the average depression score dropped from a high level to near-normal values.
- Patients with schizophrenia and bipolar disorder also showed improvement – psychotic symptoms were reduced.
- Metabolic health improved – patients lost weight, and their blood pressure, blood glucose, and triglyceride levels decreased.
The ketogenic diet may be helpful in treating depression and other psychiatric disorders, especially in individuals who do not respond well to conventional treatments. However, it is not a simple diet—it requires a high level of discipline and should only be followed under the supervision of a doctor and dietitian. It is important to emphasise that the ketogenic diet should not replace pharmacological treatment, but it can be a valuable complement to it.

Can the ketogenic diet help in treating schizophrenia?
Schizophrenia is a serious mental illness that affects thinking, emotions, and perception of reality. Symptoms such as hallucinations (e.g. hearing voices) and delusions (false beliefs) can significantly impair daily functioning. While standard treatment involves antipsychotic medication, in many cases symptoms do not fully resolve. As a result, researchers are exploring additional methods to support therapy – one of which is the ketogenic diet (Rog et al., 2024).
Studies suggest that people with schizophrenia often have impaired glucose metabolism in the brain, which may disrupt communication between nerve cells. The ketogenic diet offers an alternative energy source – ketone bodies, which can fuel the brain more effectively and improve its functioning (Rog et al., 2024).
Preliminary findings show potential benefits. In patients following keto diet the following improvements were observed:
- reduction in schizophrenia symptoms – some individuals experienced fewer hallucinations and delusions.
- improved brain function – better concentration, memory, and logical thinking were observed.
- fewer medication side effects – particularly less weight gain, a common issue with antipsychotic drugs.
better metabolic health – including lower blood glucose and lipid levels (Rog et al., 2024)
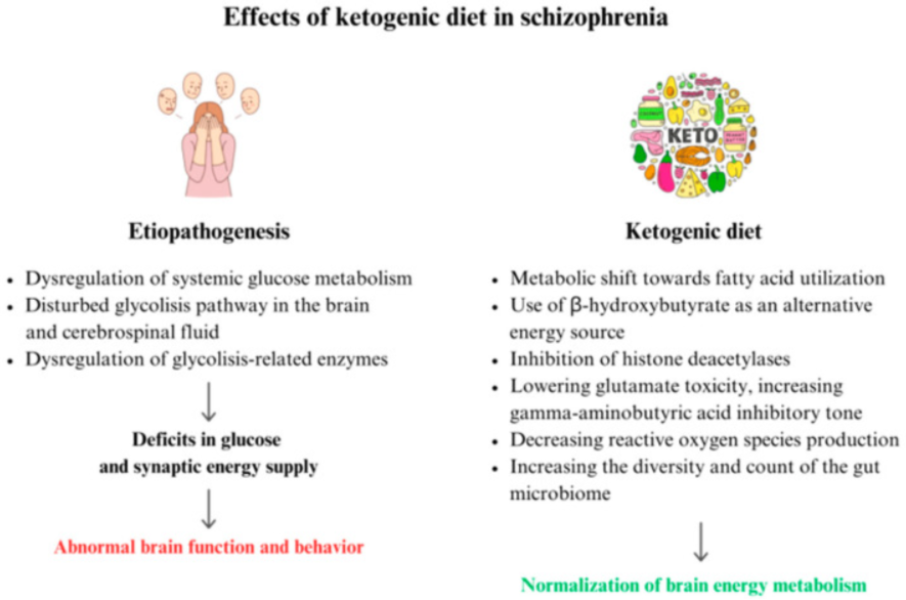
Source: https://pubmed.ncbi.nlm.nih.gov/38792361/
Despite promising research findings, the ketogenic diet is not a substitute for medication. It should not be used in place of antipsychotic treatment, but rather as a complementary approach. Any dietary change—especially one as restrictive as the ketogenic diet—must be made under the supervision of a doctor and dietitian, as sudden implementation can cause side effects. Long-term use may also lead to deficiencies in several important nutrients (Rog et al., 2024).
The ketogenic diet is a promising supportive option in the treatment of schizophrenia. It may help improve brain function, reduce symptoms, and enhance metabolic health. However, before it can be considered a standard part of treatment, more extensive research is needed.
If someone with schizophrenia is interested in trying the ketogenic diet, it is essential that they consult a healthcare professional first to ensure it is safe and appropriately managed.
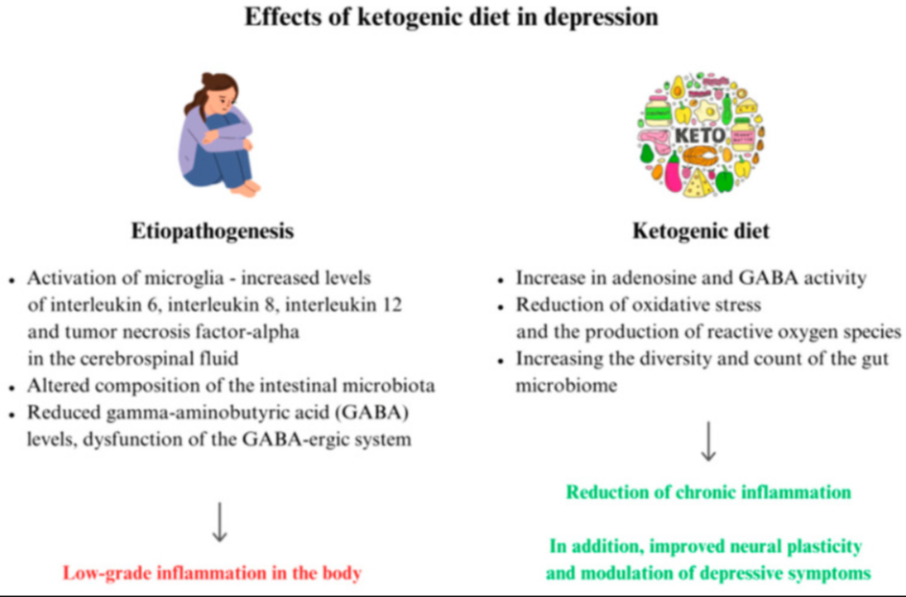
Can the ketogenic diet help in treating depression?
Researchers have observed that individuals with depression often experience impaired glucose metabolism in the brain, which may affect their mood and overall well-being. The ketogenic diet helps bypass this issue by providing energy in the form of ketone bodies, which may improve brain function and stabilise mood (Rog et al., 2024).
Studies show that ketogenic diet can help individuals suffering from depression in a few ways:
- increased energy levels – people on a ketogenic diet often report having more energy and improved concentration;
- reduced inflammation – chronic inflammation is linked to depression, and the ketogenic diet may help lower inflammatory markers;
- impact on “happiness hormones” – this diet may increase levels of GABA and serotonin, neurotransmitters that play a key role in mood regulation;
stabilised blood sugar levels – fluctuations in blood glucose can contribute to mood swings, and the ketogenic diet helps to keep these levels more stable (Rog et al., 2024).
We still have a limited number of studies assessing the role of the ketogenic diet in the treatment of depression. However, the initial findings are promising:
- Animal studies have shown that the ketogenic diet can have antidepressant-like effects, improving mood and reducing anxiety. However, this does not mean it can replace medication.
- In humans, mood improvements have been observed within just a few weeks of starting the diet.
- In some cases, patients experienced such significant improvements that they were able to reduce their medication dosage—but always under medical supervision (Rog et al., 2024).
The ketogenic diet should not be considered a replacement for antidepressant medication, but rather a complement to therapy. Any dietary change should be made under the guidance of a doctor and dietitian, to avoid side effects such as fatigue or headaches, which can occur in the initial phase of the diet (Rog et al., 2024).
The ketogenic diet is a promising approach to supporting the treatment of depression. It may help stabilise mood, enhance brain function, and increase energy levels. However, before it can be considered a standard treatment method, further research is needed. Individuals suffering from depression who are interested in trying the ketogenic diet should first consult a doctor to ensure it is a safe and appropriate option for them.
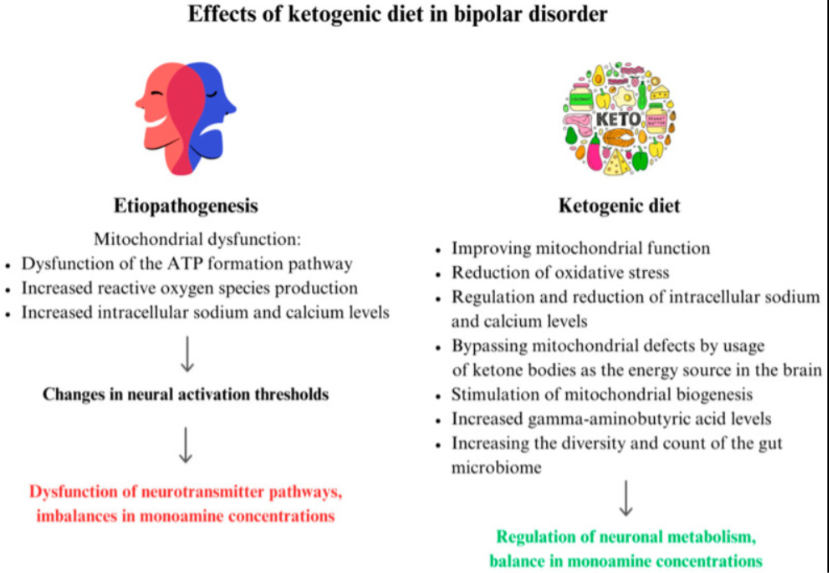
Can the ketogenic diet help in treating bipolar disorder (BD)?
Research suggests that individuals with bipolar disorder (BD) often experience mitochondrial dysfunction—issues with the „power plants” of cells that produce energy. This dysfunction may contribute to brain imbalances and sudden mood shifts. The ketogenic diet has been shown to support mitochondrial function and provide the brain with a stable energy source, which could help in managing symptoms (Rog et al., 2024).
Studies show that the ketogenic diet may help individuals suffering from BD in a few ways:
- stabilised energy levels – people with BD frequently experience extreme highs and lows in energy. The ketogenic diet may help smooth out these fluctuations;
- neurotransmitter regulation – it increases GABA (which has a calming effect) and reduces glutamate (which can contribute to overexcitement);
- reduced inflammation – chronic inflammation can affect mood and increase the risk of both depressive and manic episodes;
- stable blood sugar levels – many individuals with BD have glucose metabolism issues. The ketogenic diet helps stabilise blood glucose, which may help regulate mood swings (Rog et al., 2024)
It’s worth noting that preliminary studies have shown the following:
- In some patients following a ketogenic diet, the frequency and intensity of bipolar episodes decreased.
- Some individuals reported improved concentration and emotional stability after just a few weeks on the diet.
- In pilot studies, participants on the ketogenic diet experienced better sleep quality and overall well-being (Rog et al., 2024).
The ketogenic diet should not be considered a substitute for mood-stabilising medication, but rather a complementary therapy. Before making such a dietary change, individuals should consult both a doctor and a dietitian, as suddenly starting a ketogenic diet can cause side effects—such as fatigue or headaches—during the initial adaptation phase (Rog et al., 2024).
The ketogenic diet is a promising supportive approach for managing bipolar disorder. It may help with mood stabilisation, brain function, and energy regulation. However, more research is needed before it can be established as a standard part of treatment. Anyone living with bipolar disorder who is interested in trying the ketogenic diet should first speak with a healthcare professional to ensure it is a safe and appropriate option for their individual condition.
Does the ketogenic diet have drawbacks?
It’s important to clearly state that the ketogenic diet is not suitable for everyone. While it offers certain benefits, some individuals may experience side effects, especially in the early stages:
- fatigue, headaches, and dizziness in the first few days;
- potential nutrient deficiencies if the diet is not properly balanced;
- digestive issues, such as constipation, due to low fibre intake;
- not recommended for individuals with certain health conditions, such as liver or kidney disease.
Before starting the ketogenic diet, it is essential to consult a doctor or dietitian to ensure it is safe and appropriate for your health needs!
INTERACTIVE ACTIVITY 27
Nutritional interventions supporting glycemic stability
For many clients, it is neither necessary nor realistic to learn the exact glycemic index (GI) or glycemic load (GL) of each food item. However, it is useful to understand the basic principles of how different carbohydrates affect blood sugar levels.
The glycemic index describes how quickly carbohydrates in a given food raise blood glucose levels. The higher the index, the faster the blood sugar spike. Foods with a high GI (e.g., white bread, sugary drinks, processed cereals) cause a rapid increase in glucose levels, while foods with a low GI (e.g., whole grains, legumes, vegetables) are digested more slowly and contribute to better glycemic stability.
When planning healthy meals, the glycemic index (GI) is often discussed. However, it’s also important to consider the glycemic load (GL), which accounts not only for the type of food but also the amount of carbohydrates in a given portion. GL better reflects the real impact a full meal has on blood glucose.
- GI tells us about the quality of carbohydrates (i.e., whether they are digested quickly or slowly).
- GL also considers the quantity of carbohydrates – i.e., the actual glycemic impact of a portion.
| Product | GI | Carbohydrate Content | Glycemic Load (GL) | Comment |
| Watermelon (1 slice, 120 g) | High (~75) | Low (~6 g) | Low (~4–5) | Despite high GI, low sugar content → low GL |
| White rice (1 portion, 150 g) | High (~70) | High (~45 g) | High (~30–35) | High carb content → significant effect on blood glucose |
Conclusion:
Watermelon has a high GI but a low GL – so it doesn’t need to be avoided.
White rice has both a high GI and a high GL – it’s better to limit it or combine it with fiber and protein.
Example 2: Two breakfasts – which is better?
| Meal | GI | GL | Glycemic Response |
| White bread roll with jam | High | High | Quick sugar spike, hunger returns after 1–2 h |
| Oatmeal with milk and nuts | Low–medium | Low | Stable blood sugar, lasting satiety |
In practice, it’s best to choose meals with a low or moderate glycemic load, as they promote longer-lasting fullness, reduce glycemic fluctuations, and support better concentration.
Practical Tips for Health Professionals:
You don’t need to memorize all the numbers. It’s enough to remember:
- GI refers to the type of carbohydrate,
- GL considers both amount and serving size,
- Highly processed foods and those rich in simple sugars often have high GL – but this depends on both GI and typical portion size,
- Combining carbs with fiber, protein, or fat lowers the GL of the overall meal.
If in doubt, it’s advisable to consult a qualified dietitian who can tailor recommendations to the client’s health status and lifestyle.
| Bibliography |
| Danan, A., Westman, E. C., Saslow, L. R., & Ede, G. (2022). The ketogenic diet for refractory mental illness: A retrospective analysis of 31 inpatients. Frontiers in Psychiatry, 13, 951376. https://doi.org/10.3389/fpsyt.2022.951376 Gao, M., Kirk, M., Lash, E., Knight, H., Michalopoulou, M., Guess, N., Browning, M., Weich, S., Burnet, P., Jebb, S. A., Stevens, R., & Aveyard, P. (2024). Evaluating the efficacy and mechanisms of a ketogenic diet as adjunctive treatment for people with treatment-resistant depression: A protocol for a randomised controlled trial. Journal of Psychiatric Research, 174, 230–236. https://doi.org/10.1016/j.jpsychires.2024.04.023 Grajek, M., Krupa-Kotara, K., Białek-Dratwa, A., Sobczyk, K., Grot, M., Kowalski, O., & Staśkiewicz, W. (2022). Nutrition and mental health: A review of current knowledge about the impact of diet on mental health. Frontiers in Nutrition, 9, 943998. https://doi.org/10.3389/fnut.2022.943998 |
